Resistance to colistin, a so-called antibiotic of last resort, has been found in both bacteria and pigs in the UK.
Tests carried out by Public Health England have found colistin resistance in 15 of 24,000 bacterial samples – including Salmonella and E Coli – it had kept on record from cases between 2012 and 2015. The Animal and Plant Health Agency (APHA), meanwhile, has discovered colistin-resistant bacteria in samples from three pig farms.
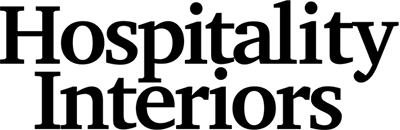
The APHA started screening archived isolates and biological samples after a report from China described the discovery of transferable colistin resistance in E coli from pigs, raw meat and humans. Chinese scientists identified the presence of a gene – mcr-1 – that can rapidly spread resistance between species.
Isolates of E coli collected from pigs in 2013 and 2015 as part of Government surveillance were screened by the APHA and none were found to carry the gene, but then stored pig caeca collected throughout 2015 were defrosted and the contents cultured on selective media containing colistin to increase the sensitivity of detection. The mcr-1 gene was identified in E coli from one sample.
E coli recovered from clinical diagnostic investigation in England and Wales were also screened. Isolates originating from two separate farms were found to be positive for the mcr-1 gene.
The Veterinary Medicines Directorate, which oversaw the testing, said the bacteria identified with the mcr-1 gene were found to be susceptible to many other antibiotics.
Colistin, which has been used sparingly in human health here to try and retain its potency, has been used more widely in agriculture. Figures obtained by the Alliance to Save Our Antibiotics suggest 837kg of colistin was sold to British farms in 2014, while 300kg was prescribed by doctors.
Throughout Europe, 500t of colistin is said to have been used on farms in 2014 compared to 1t in human health. Spain (177t); Italy (133t); Germany (124t) and France (50t) were particularly large consumers of the antibiotic.
Professor Alan Johnson from Public Health England said the organisation’s assessment was that the public health risk posed by this gene was currently considered very low, but was subject to ongoing review as more information became available.
“The organisms identified can be killed by cooking your food properly and all the bacteria we identified with this gene were responsive to other antibiotics, called carbapenems,” he said. “We will monitor this closely, and will provide any further public advice as needed.”
In early December, The Responsible Use of Medicines in Agriculture Alliance (RUMA) announced voluntary restrictions by vets on the use of colistin in UK livestock. The move came pending the results of a risk assessment to be carried out by the European Commission, and colistin use will be restricted to an antibiotic of last resort and will be used only after susceptibility testing had shown it was the only effective antibiotic available for treating the sick animals.